Estimated reading time: 8 minutes
When brushing teeth feels like a battle, homework ends in tears, and even getting dressed sparks a meltdown, it’s not your fault. It may be Pathological Demand Avoidance (PDA).
Many parents of children with Pathological Demand Avoidance (PDA) describe feeling exhausted and frustrated. It’s misunderstood by others who assume it’s “bad behavior.”
But here’s the truth: PDA is not defiance. It’s an anxiety-driven profile of autism where ordinary demands can feel overwhelming and trigger the fight-flight-freeze response.
When we understand this, everything changes. It’s because behavior is communication, and calmer brains can cooperate.
In this guide, you’ll learn:
- What PDA looks like in everyday life
- Why kids with PDA resist demands
- 13 science-backed Pathological Demand Avoidance Strategies to support your child at home and school
- Practical examples, parent stories, and expert insights to help you feel empowered
What is Pathological Demand Avoidance (PDA)?
Pathological Demand Avoidance (PDA) is a profile of autism spectrum disorder (ASD). It’s characterized by extreme demand avoidance rooted in anxiety and nervous system dysregulation.
Children with PDA may appear imaginative and socially aware. But everyday requests can trigger panic-like responses.
Key characteristics include:
- Extreme avoidance of ordinary demands
- Excessive mood swings and impulsivity
- Use of humor, excuses, or role play to avoid tasks
- A strong need for control to feel safe
Important to remember: PDA is not intentional misbehavior. It’s the brain saying, “This feels too much.”
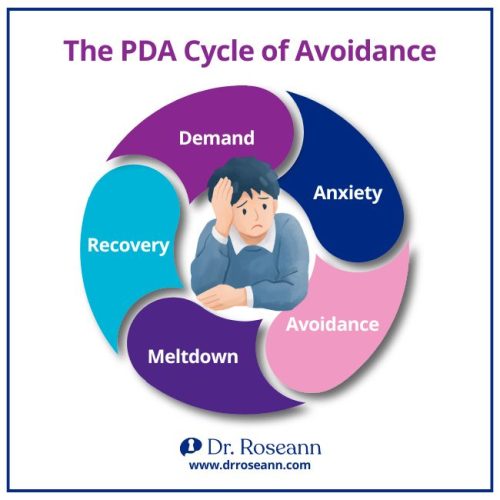
Why Do Kids With PDA Resist Demands?
For kids with PDA, even ordinary demands feel like threats.
- The amygdala (fear center) in the brain gets triggered.
- Their body shifts into fight, flight, or freeze.
- Avoidance becomes a way to regain control and reduce anxiety.
“PDA is not about willful disobedience. It’s an anxiety-driven response to demands that feel overwhelming.” – Dr. Elizabeth Newson, psychologist and PDA researcher
How is PDA Different From ODD?
Parents often confuse PDA with Oppositional Defiant Disorder (ODD). It’s because both involve refusal behaviors. But the root causes are different:
- ODD: Pattern of persistent defiance and anger toward authority figures.
- PDA: Avoidance driven by anxiety and dysregulation, not defiance.
If your child is cooperative when calm but melts down when pressured, it may be PDA, not ODD.
| Pathological Demand Avoidance (PDA) | Oppositional Defiant Disorder (ODD) |
|---|---|
| Root cause: Anxiety + nervous system dysregulation | Root cause: Defiance + oppositional patterns |
| Demand avoidance is anxiety-driven | Refusal is intentional and oppositional |
| Child often wants to cooperate but feels overwhelmed | Child resists to assert independence/authority |
| Avoids tasks using distraction, excuses, humor, or role play | Argues, refuses, or deliberately annoys others |
| Extreme fight-flight-freeze responses to ordinary demands | Pattern of anger, irritability, and defiance toward authority |
| High social awareness + creativity but struggles with demands | Less focus on social strategies; more outward defiance |
| Responds best to reduced demands, choices, and collaboration | Responds best to clear boundaries, consistent discipline |
13 Pathological Demand Avoidance Strategies
Parenting a child with PDA requires a unique balance of empathy, flexibility, and structure. Here are 13 brain-based strategies that really help.
1. Recognize Sensory Issues
Many children with PDA have sensory sensitivities. Minimize overwhelming stimuli (noise, bright lights). You can also provide comfort tools (weighted blankets, noise-canceling headphones).
2. Person-Centered Communication
- Use clear, concise language (“Room. Teeth. Pajamas.”).
- Give extra processing time before repeating requests.
- Provide visual schedules with icons or pictures.
- Offer choices to increase a sense of control.
- Reinforce effort with specific praise (“You did a great job brushing your teeth!”).
3. Implement Predictability and Routine
Children with PDA thrive on structure. Share changes in advance as surprises often trigger resistance.
4. Provide Coping Strategies
Teach tools like:
- Deep breathing
- Mindfulness
- Sensory breaks
Collaborate with therapists to help your child practice when calm.
5. Encourage Social Skills Development
Support your child through:
- Structured playdates
- Social groups
- Role play practice
6. Flexibility in Demands
Balance routine with flexibility. If your child is overwhelmed, adjust expectations and allow breaks.

7. Promote Independence
Give your child small responsibilities (choosing clothes, packing a backpack). Celebrate effort and progress.
8. Build a Supportive Network
Share information about PDA with teachers, therapists, and extended family. This way, everyone is on the same page.
9. Emphasize Natural Solutions for Brain Health
- Nutritious diet
- Regular exercise
- Mindfulness or yoga
These support attention, mood, and resilience.
10. Celebrate Small Victories
Acknowledge small wins. Success builds confidence and reduces demand avoidance.
11. Role Play and Social Strategies
Practice scenarios like:
- Asking for help at school
- Trying a new activity
- Handling unexpected changes
This reduces anxiety and builds confidence.
12. Long-Term Planning for Future Success
- Collaborate on IEPs (Individualized Education Program).
- Plan transitions between grades.
- Explore post-school goals early.
13. Addressing School Challenges Effectively
- Advocate for classroom accommodations (sensory breaks, extended time).
- Create individualized behavior plans.
- Monitor progress regularly.
How to support your child during meltdowns
When a PDA meltdown happens:
- Stay calm—your regulation helps theirs.
- Remove demands and let the storm pass.
- Offer sensory comfort.
- Use a few words; reassure with presence.
Parent story: Mark’s son exploded over homework. Instead of arguing, Mark quietly sat near him. Later, his son whispered, “Thanks for not yelling.” That moment showed him connection mattered more than compliance.
Common Mistakes Parents Must Avoid
- Rigid rules → escalate anxiety.
- Overexplaining in the moment → the child can’t process.
- Labeling as “lazy” or “defiant” → increases shame.
Takeaway: It’s not bad parenting—it’s a dysregulated brain.
PDA Success Stories
When I first met Emilio, a bright 12-year-old with Pathological Demand Avoidance, he carried himself with a quiet but firm resistance—arms crossed, eyes avoiding mine, as if to say, “Don’t ask me to do anything.” His mom, Celeste, was exhausted from the daily battles. She had tried everything she knew—pleading, negotiating, even giving in—yet Emilio seemed to push back harder each time.
In our BrainBehaviorReset™ Program, the first step wasn’t about fixing Emilio but helping Celeste learn how to hold steady. Once she began staying consistent, modeling calm, and giving him choices he could manage, Emilio slowly started to trust that she wasn’t there to control him.
The changes were gradual but real. Instead of spiraling into avoidance the moment a demand was placed, Emilio began reaching for the coping tools we practiced. Small wins stacked up, and Celeste noticed she was no longer locked in constant battles. With relief in her voice, she told me, “For the first time, I don’t feel like I’m fighting him every day.”
Stories like Emilio’s remind us: progress is possible.
Finding Hope with Pathological Demand Avoidance Strategies
Parenting a child with PDA is hard. There’s no sugarcoating it.
But the good news is, you’re not alone and there are tools that work. With the right Pathological Demand Avoidance strategies, you can calm your child’s brain, reduce power struggles, and bring more peace to your home.
Remember:
- Behavior is communication.
- It’s not bad parenting—it’s a dysregulated brain.
- Small wins add up to big progress.
Want more support? Download our Free PDA Parenting Checklist today and start creating calmer, more cooperative routines.
FAQs About Pathological Demand Avoidance Strategies
Can Pathological Demand Avoidance strategies really help?
Yes. They don’t “fix” PDA, but they lower anxiety and reduce meltdowns by calming the brain and giving your child tools to cope.
What are the best Pathological Demand Avoidance strategies for routines?
Use visual schedules, choices, and small rewards. These make daily routines less overwhelming and more predictable.
How are Pathological Demand Avoidance strategies different from discipline?
Discipline focuses on consequences. PDA strategies focus on reducing demands, staying flexible, and calming anxiety.
Do Pathological Demand Avoidance strategies work at school?
Yes. With teacher support and an IEP or accommodations, kids can thrive using the same strategies—like breaks, choices, and reduced pressure.
Terminology
- PDA (Pathological Demand Avoidance): A profile of autism with extreme demand avoidance.
- Fight-flight-freeze: Automatic stress response when the brain perceives a threat.
- ODD (Oppositional Defiant Disorder): A behavior disorder with persistent defiance toward authority.
- Self-regulation: The ability to manage emotions, energy, and behavior.
- IEP (Individualized Education Program): A legal plan in U.S. schools that outlines special education services, supports, accommodations, and goals tailored to a child’s unique needs.
Citations:
O’Nions, E., Gould, J., Christie, P., Gillberg, C., Viding, E., & Happé, F. (2015). Identifying features of “pathological demand avoidance” using the Diagnostic Interview for Social and Communication Disorders (DISCO). European Child & Adolescent Psychiatry, 25(4), 407–419. https://doi.org/10.1007/s00787-015-0740-2
Shanmugam, H., Ganguly, S., & Priya, B. (2021). Plant food bioactives and its effects on gut microbiota profile modulation for better brain health and functioning in Autism Spectrum Disorder individuals: A review. Food Frontiers. https://doi.org/10.1002/fft2.125
Yasinski, C., Hayes, A. M., Ready, C. B., Abel, A., Görg, N., & Kuyken, W. (2019). Processes of change in cognitive behavioral therapy for treatment-resistant depression: psychological flexibility, rumination, avoidance, and emotional processing. Psychotherapy Research, 30(8), 1–15. https://doi.org/10.1080/10503307.2019.1699972
Always remember… “Calm Brain, Happy Family™”
Disclaimer: This article is not intended to give health advice and it is recommended to consult with a physician before beginning any new wellness regime. The effectiveness of diagnosis and treatment vary by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!
© Roseann Capanna-Hodge