Estimated reading time: 6 minutes
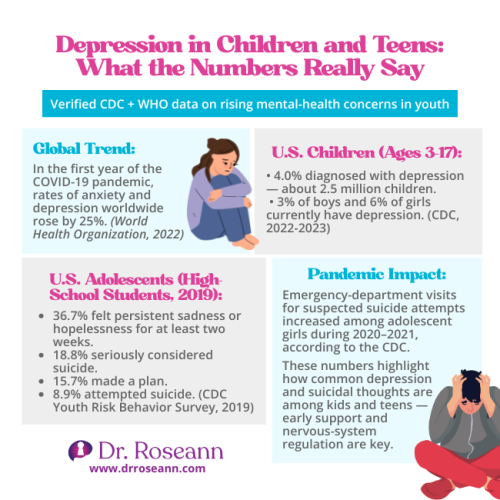
Recognizing the early signs of mood disorder symptoms in children can be the difference between years of struggle and getting your child the help they need to thrive.
Some days it feels like you’re watching your child battle storms you can’t see: and you’re desperately searching for ways to throw them a lifeline.
If you’ve been noticing changes in your child’s emotions, behavior, or overall well-being that feel bigger than typical ups and downs, you’re not imagining things. Mood disorder symptoms in children can be subtle at first, but they’re real, treatable, and most importantly: not your fault.
As a mental health expert who’s worked with thousands of families over 30+ years, I want you to know that early recognition is one of the most powerful tools you have. When we understand what we’re seeing, we can respond with the right support instead of wondering if we’re overreacting or missing something crucial.
Here’s what every parent needs to know about recognizing childhood mood disorders, teen depression symptoms, and when it’s time to seek professional help to improve mood, depression, and the like.
What Are the Most Common Mood Disorder Symptoms in Children and Teens?
Mood disorder symptoms in young people often look different from what you might expect. Instead of just sadness, you’re more likely to see irritability in children, explosive anger, or complete emotional shutdown.
The most common signs include:
| Symptom domain | Examples you might see | What to track |
|---|---|---|
| Emotional | Persistent sadness Extreme mood swings Tearfulness Loss of interest hopelessness/low self-worth |
Frequency/duration Loss of pleasure Intensity vs. trigger |
| Behavioral | Emotional dysregulation Withdrawal Sleep changes Appetite changes Trouble concentrating or deciding |
Impact on schoolwork, friendships, and family routines |
| Physical | Headaches/stomachaches Fatigue Restlessness or slowed movements |
Rule out medical causes Patterns with stress or school days |
Remember, behavior is communication. These symptoms aren’t defiance: they’re your child’s nervous system telling you it’s overwhelmed and needs support.
How Do I Know If My Child’s Mood Changes Are Normal or Something More Serious?
This is the question that keeps so many parents awake at night. The key difference lies in intensity, duration, and impact on daily functioning.
Normal mood fluctuations:
- Last a few days to a week
- Have clear triggers (disappointment, stress, changes)
- Don’t significantly interfere with school, friendships, or family life
- Your child can still experience joy and engage in activities
Concerning mood changes:
- Persist for weeks or months
- Seem disproportionate to circumstances
- Impact academic performance, relationships, or daily activities
- Include thoughts of self-harm or feeling like life isn’t worth living
Hannah, a mom I worked with, noticed her 9-year-old’s “bad days” were becoming “bad weeks.” What started as occasional grumpiness evolved into daily tears, refusing to go to school, and saying things like “I’m stupid and nobody likes me.” That’s when she knew it was time to dig deeper.
Trust your parental instincts. You know your child better than anyone, and if something feels different for more than two weeks, it’s worth exploring.
What’s the Difference Between Mood Disorder Symptoms in Kids vs. Adults?
Children and teens express mood disorders very differently than adults, which is why these conditions often go unrecognized or misdiagnosed.
In children (ages 6-12):
- Irritability and anger are more common than sadness
- Physical complaints like headaches and stomachaches
- Regression in behaviors (bedwetting, clinginess)
- Difficulty separating from parents
- Academic problems or school refusal
In teens (ages 13-18):
- More likely to show classic depression symptoms like persistent sadness
- Risky behaviors or substance experimentation
- Extreme mood swings and emotional volatility
- Social withdrawal or complete isolation
- Sleep disturbances (sleeping too much or too little)
Brain Science Spotlight
Recent research reveals that childhood mood disorders involve disrupted neural pathways between the emotional centers of the brain (amygdala) and the thinking brain (prefrontal cortex). Dr. Joan Luby, lead researcher on childhood depression studies, indicates that depression in children is associated with measurable changes in brain structure and function, particularly in areas responsible for emotional regulation. (Kerestes et al., 2014; Luby et al., 2013)
This discovery helps us understand why traditional talk therapy alone often isn’t enough. When the nervous system is dysregulated, children can’t access the thinking parts of their brain needed for emotional processing. This isn’t willful defiance: it’s neurobiology in action.
What this means for your family: We need to calm the brain first before expecting emotional or behavioral change to stick.
When Should I Be Concerned About My Child’s Emotional Outbursts?
Every child has meltdowns: but when do those big emotions signal something more serious?
Typical emotional outbursts:
- Have identifiable triggers
- Last 10-30 minutes
- Child can be comforted or redirected
- Happen occasionally, not daily
- Don’t result in harm to self or others
Concerning emotional dysregulation:
- Occur multiple times daily or weekly
- Last hours or trigger doesn’t match intensity
- Child seems “unreachable” during episodes
- Include threats of self-harm or harming others
- Significantly disrupt family life or school functioning
Based on pediatric mental health guidance (Birmaher et al., 2007; National Institute of Mental Health, 2023).
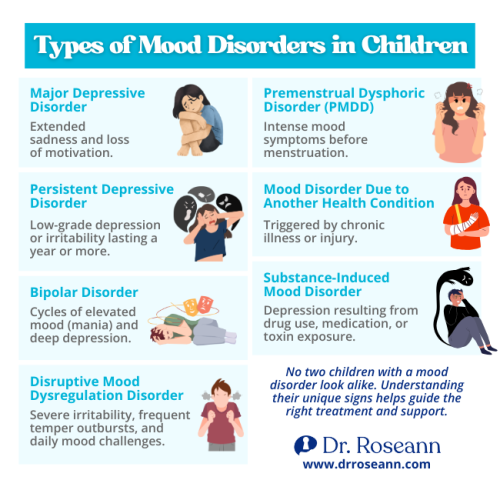
How Can I Tell if My Teen Has Depression vs. Just Typical Teenage Moodiness?
The teenage years naturally come with emotional ups and downs, but teen depression symptoms go far beyond typical adolescent mood swings.
| Feature | Typical teen mood | Possible depression |
|---|---|---|
| Social behavior | Some family withdrawal; maintains friendships | Pulls away from friends and activities |
| Sleep | Variable but within usual range | Insomnia or sleeping 10–12+ hours regularly |
| School | Generally on track | Noticeable drop in grades or attendance |
| Interest/pleasure | Still enjoys some hobbies | Loss of interest in most or all activities |
| Thoughts/feelings | Irritable but rebounds | Hopelessness; thoughts of death/self-harm |
Eli, a 16-year-old I worked with, went from being a social, athletic kid to sleeping 12+ hours a day, skipping school, and telling his parents “nothing matters anymore.” That’s when his family knew this was more than teenage angst.
Dr. Roseann’s Therapist Tip
In my 30+ years of clinical practice, I’ve learned that the most important thing parents can do is regulate themselves first. Here’s what I tell parents: When you stay calm in the face of your child’s emotional outbursts, you’re literally helping their nervous system learn how to regulate.
Try this today: The next time your child is dysregulated, take three deep breaths before responding. Your calm energy gives their overwhelmed nervous system something to match.
Why it works: Parental regulation influences child by behavioral modeling, not just mirror neurons. When you model regulation, you’re teaching their brain how to find calm.
Remember: It’s gonna be OK. Every small moment of co-regulation builds your child’s capacity for self-regulation over time.
What Should I Do When I Notice These Warning Signs?
First, take a deep breath. Recognizing mood disorder symptoms in your child doesn’t mean you’ve failed as a parent: it means you’re being proactive about getting them help.
Immediate steps:
- Document patterns – Note triggers, duration, and intensity of symptoms
- Rule out medical causes – Schedule a pediatric check-up
- Reach out to school – Ask teachers if they’ve noticed changes
- Seek professional evaluation – Contact a mental health professional who specializes in pediatric mood disorders
- Focus on nervous system regulation – Start implementing calming routines
Long-term support strategies:
- Create predictable daily routines
- Limit screen time and prioritize sleep
- Incorporate co-regulation activities like deep breathing together
- Consider dietary changes that support brain health
- Build a support network of understanding professionals and parents
How Do Mood Disorders Show Up Differently in School-Age vs. Teen Years?
Understanding developmental differences in childhood mood disorders helps you know what to look for at each stage.
| Age group | Common presentations | Notes for parents/teachers |
|---|---|---|
| 6–10 years | Somatic complaints; irritability/anger; regression; separation difficulty; school avoidance | Kids may lack words for feelings—watch behavior and body complaints |
| 11–13 years | More “adult-like” depression signs; peer conflicts; academic dips; bigger mood swings | Hormonal shifts can amplify dysregulation; routines help |
| 14–18 years | Classic depression symptoms; substance experimentation; relationship strain; future worries; suicidal talk | Increased risk-taking requires closer monitoring and support |
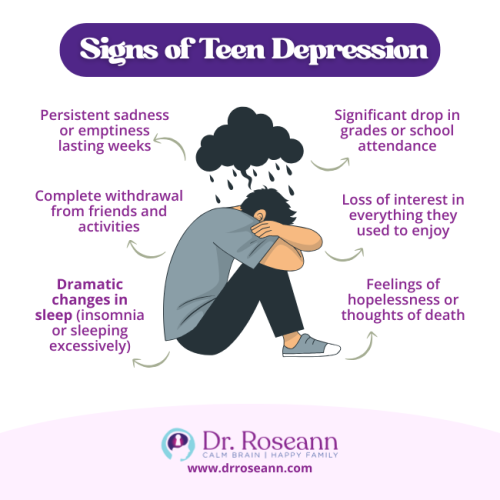
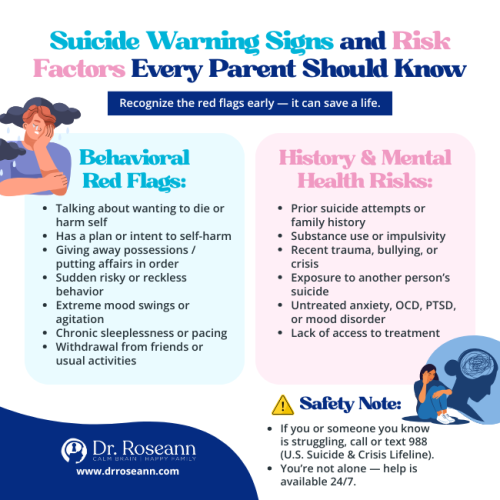
What Are the Red Flags That Require Immediate Professional Help?
Some symptoms require urgent attention and cannot wait for a regular appointment.
Seek immediate help if your child:
- Expresses thoughts of suicide or death
- Engages in self-harm behaviors
- Shows signs of psychosis (hearing voices, seeing things)
- Has dramatic personality changes overnight
- Stops eating or drinking for extended periods
- Becomes completely non-functional for days
Contact emergency services or go to the ER if:
- Your child has a specific suicide plan
- They’ve made a suicide attempt
- You find evidence of self-harm
- They’re threatening to hurt others
- You’re genuinely afraid for their safety
Remember: You are not alone in this journey. There are professionals trained specifically to help families navigate mood disorders in children and teens.
Moving Forward With Hope
Recognizing mood disorder symptoms in children can feel overwhelming, but it’s actually the first step toward getting your child the support they need. Early intervention makes an enormous difference in outcomes, and with the right approach, children with mood disorders can absolutely thrive.
Remember these key points:
- Symptoms that persist for weeks deserve professional attention
- Your child’s brain can learn regulation with proper support
- Behavior is communication: listen to what it’s telling you
- You’re the expert on your own child: trust your instincts
- Help is available, and recovery is absolutely possible
The journey might feel daunting right now, but thousands of families have walked this path and found their way to calmer, happier days. With understanding, support, and the right interventions, your child can learn to regulate their emotions and rediscover joy.
Ready to take the next step? Download our comprehensive Natural Mood and Behavior Regulation Kit for supporting children with mood challenges. Inside, you’ll find practical strategies for daily regulation, scripts for talking with your child about their emotions, and a step-by-step guide for finding the right professional help. This isn’t about quick fixes: it’s about building lasting skills for emotional wellness.
Read more about: Typical Moodiness vs. Childhood Depression
FAQs
How early can mood disorders be diagnosed in children?
While mood symptoms may emerge as early as preschool age, reliable diagnosis of mood disorders in children under age 5 is challenging and uncommon due to developmental variability and overlap with normal childhood behaviors. More accurate diagnosis is often made in school-age children and adolescents.
Can mood disorders in children be cured?
While mood disorders are typically managed rather than “cured,” with proper treatment including nervous system regulation, therapy, and sometimes medication, children can learn effective coping strategies and lead fulfilling lives.
Do mood disorders always require medication?
Not necessarily. Many children benefit from therapy, lifestyle changes, neurofeedback, and nervous system regulation techniques. Medication decisions should always be made in consultation with qualified mental health professionals.
How long does treatment typically take?
Treatment timelines for mood disorders in children and teens can vary substantially. While some may experience improvement within several weeks of evidence-based therapy or intervention, others may require more time, adjustments, or combined medical approaches. Building lasting emotional regulation skills is typically a 6-12 month process.
Can parents cause mood disorders in their children?
Mood disorders are influenced by genetics, neurobiology, and environmental stressors; while parenting practices can affect symptom expression and a child’s resilience, no single factor solely determines risk. Rarely, chronic severe adversity in the home can contribute to mood symptoms but is not considered the primary cause.
Citations
Birmaher, B., Brent, D., & The AACAP Work Group on Quality Issues. (2007). Practice parameter for the assessment and treatment of children and adolescents with depressive disorders. Journal of the American Academy of Child & Adolescent Psychiatry, 46(11), 1503–1526. https://doi.org/10.1097/chi.0b013e318145ae1c
Kerestes, R., Davey, C. G., Stephanou, K., Whittle, S., & Harrison, B. J. (2014). Functional brain imaging studies of youth depression: A systematic review. NeuroImage: Clinical, 4, 209–231. https://doi.org/10.1016/j.nicl.2013.11.009
Luby, J. L., Belden, A. C., Harms, M. P., Tillman, R., & Barch, D. M. (2013). Preschool is a sensitive period for the influence of depression on the neural circuitry of emotion. JAMA Psychiatry, 70(9), 983–990. https://doi.org/10.1001/jamapsychiatry.2013.80
National Institute of Mental Health. (2023). Depression in children and adolescents. https://www.nimh.nih.gov/health/publications/depression-in-children-and-adolescents
Thapar, A., Collishaw, S., Pine, D. S., & Thapar, A. K. (2012). Depression in adolescence. The Lancet, 379(9820), 1056–1067. https://doi.org/10.1016/S0140-6736(11)60871-4
Zuckerbrot, R. A., Cheung, A. H., Jensen, P. S., Stein, R. E. K., & Laraque, D., for the GLAD-PC Steering Group. (2018). Guidelines for Adolescent Depression in Primary Care (GLAD-PC): Part I. Pediatrics, 141(3), e20174081. https://doi.org/10.1542/peds.2017-4081
Always remember… “Calm Brain, Happy Family™”
Disclaimer: This article is not intended to give health advice and it is recommended to consult with a physician before beginning any new wellness regime. *The effectiveness of diagnosis and treatment vary by patient and condition. Dr. Roseann Capanna-Hodge, LLC does not guarantee certain results.
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!
©Roseann Capanna-Hodge