Estimated reading time: 7 minutes
When a capable young adult freezes on the runway of life, it’s rarely laziness. It’s usually young adult depression, anxiety, and a dysregulated nervous system hijacking forward momentum.
If your young adult is stuck at home, avoiding school or work, and bristling at responsibility, you’re not alone—and you’re not a “bad” parent. What’s often labeled failure to launch is, in my experience, an emotional dysregulation. It’s also skill gaps and family patterns that accidentally keep everyone stuck.
The good news: when we calm the brain first, teach skills, and reset communication, change follows.
In this guide, you’ll learn:
- What failure to launch is (and isn’t)
- How young adult anxiety and depression fuel avoidance,
- The role of screen time and mental health,
- And more
What Is “Failure to Launch”… and What Is It Not?
Failure to launch isn’t a clinical diagnosis. It’s a cluster of patterns where a young adult remains dependent on parents and avoids steps toward independence.
Think of stalled schooling or work, and social withdrawal. Add low stress tolerance and heavy reliance on parent structure instead of internal skills.
What it’s not: laziness, moral failing, or just “bad motivation.” Most of these kids want independence. But, they don’t yet have the regulatory and executive functioning skills to face discomfort and persist.
Parent snapshot: “Evan, 21, quit two jobs in a semester. He wasn’t ‘unmotivated’—he panicked in new situations and shut down.”
Takeaway: Behavior is communication. When we stabilize the nervous system, capacity grows.
Why Do Anxiety and Depression Wire the Brain for Avoidance?
Most lifetime mental health conditions start before age 24. It means many failure-to-launch stories began in childhood. This is even if symptoms were quiet or masked by structure (Kessler et al., 2005).
Two patterns often show up:
- Internalizers: worry loops, perfectionism, shutdowns; they can look “fine” yet feel hopeless.
- Externalizers: irritability, anger, “I don’t care”; easier to spot but often misunderstood.
When the nervous system is revved or collapsed, the brain prioritizes escape over engagement. So school, work, and even chores feel unsafe.
That’s why my framework is Regulate → Connect → Correct (Regulate. Connect. Correct.™): calm the brain first, then build skills and accountability.
“You can’t teach a dysregulated brain—regulate first, then skills stick.”
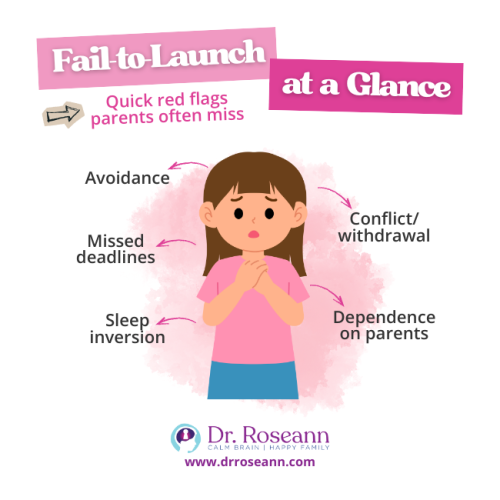
How Do I Spot the Hidden Signs at Home?
Look for patterns, not one-offs:
- Academic/work avoidance: dropped classes, missed shifts, perfectionism → paralysis
- Emotional dysregulation: blow-ups or shutdowns after small asks
- Executive skill gaps: time blindness, task initiation problems, messy planning
- Sleep/screen spirals: late nights, fatigue, missed mornings
- Parent accommodation: doing tasks for them, walking on eggshells to avoid explosions
Parent story:
Siena’s 19-year-old with ADHD slept all day and gamed all night. Once Siena reduced “rescue” behaviors and we taught executive functioning skills with co-regulation, her son slowly took over mornings and started a part-time job.
Takeaway: Reduce parent accommodation while increasing support for skill-building.
Are Screens Quietly Amplifying the Problem?
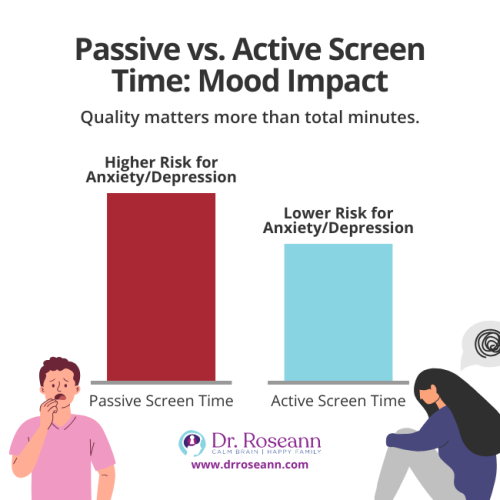
Not all screen time is equal. Passive scrolling is linked with more depressive symptoms, while active, connected use can be less risky (Twenge et al., 2018).
For dysregulated young adults, passive use often replaces real-world practice with peers and responsibilities. It fuels avoidance and isolation.
Try this:
- Set device boundaries tied to daily responsibilities (sleep, chores, tasks).
- Swap 30–60 minutes/day of passive scrolling for active engagement (creating, connecting) or movement.
Parent snapshot:
Ravi, 22, spent 8+ hours gaming. We shifted one hour to a peer job-search group and 20 minutes to a walk. Anxiety dipped; he sent three applications that week.
What Family Patterns Keep Kids Stuck—And How Do We Reset Them?
Families understandably accommodate to reduce explosions or shutdowns. Over time, that can reinforce avoidance. Family factors can maintain impairment (see OCD literature illustrating family accommodation and functioning burdens; Storch et al., 2014).
Reset with “Regulate → Connect → Correct”:
- Regulate (Co-regulation first): Breathe, ground, then speak. Your calm body cues your child’s nervous system to settle.
- Connect (Validate): “I see this is hard. I’m with you.”
- Correct (Clear limits + choices): “You can game after you apply to one job. Need help breaking it down?”
Micro-scripts (use verbatim):
- “I’m going to slow my voice. Let’s take 3 breaths together, then plan your morning.”
- “Do you want to start with laundry or emailing your advisor? I’ll sit nearby for 10 minutes.”
Behavior is communication. Decode it, then teach the missing skill.
What Actually Works to Move a Failure to Launch Young Adult Forward?
Talk therapy alone can help gain insight. But regulation-first methods often unlock real-world change faster for stuck young adults:
Science-Backed Tools (what we use in BrainBehaviorReset)
- QEEG brain map to see patterns of over/under-activation that correlate with anxiety, mood, and focus challenges
- Neurofeedback for anxiety to train brainwaves toward stability
- PEMF therapy to support downshifting a revved nervous system
- Coaching on executive functioning skills (initiation, planning, time management)
- Independent living skills (sleep routine, money basics, transportation) layered in small, repeatable steps
Mini case:
Maya, 20, paused college after panic attacks. QEEG revealed high fast-wave activity; neurofeedback, combined with sleep and exposure coaching, reduced panic. She returned part-time the next term.
Start This Week: A Simple 7-Day Plan
Small wins build confidence. Try this:
- Day 1–2 (Regulate): 5-minute breath + 10-minute walk together; bedtime moved 30 minutes earlier.
- Day 3 (Connect): Validate the hardest task; co-create a 20-minute “first step.”
- Day 4 (Correct): Tie privilege to task: “Apply to one job → phone after dinner.”
- Day 5 (Skills): Teach a time-boxing method (two 25-minute work blocks + 5-minute breaks).
- Day 6 (Practice): One household task becomes their job (laundry or dishes), coached—not rescued.
- Day 7 (Reflect): Review wins, tweak barriers, schedule next week’s repeats.
Pro tip: Keep asks small, specific, and scheduled. The nervous system loves predictability.
Holding Hope and Boundaries (When Progress Feels Slow)
Change is rarely linear. Expect spurts and stalls. Remember, it’s not bad parenting—it’s a dysregulated brain. Your job is to bring the calm, hold loving limits, and keep practicing Regulate → Connect → Correct.
Key Encouragements
- Your calm is medicine. Co-regulation beats lectures.
- Track tiny wins. “Out of bed by 10,” “sent one email,” “took a walk.”
Get skilled help. If failure to launch is straining your family, it’s OK to ask for a science-backed plan.
In a Nutshell: Calm Brain, Forward Momentum
Failure to launch is a solvable brain-and-behavior puzzle. When we regulate first, connect with empathy, and then correct with clear, consistent steps, young adults build the skills and confidence to take off.
You’re not alone—and it’s going to be OK.
Next step: Want help mapping your child’s plan? Explore our BrainBehaviorReset® supports or read my guide on co-regulation and executive skills to get started today.
FAQs
Is “failure to launch” a diagnosis?
No. It’s a descriptive label for stuck patterns. The why often includes anxiety, depression, ADHD, or skill gaps.
How is this connected to early mental health?
Many issues begin before adulthood; three-quarters of lifetime cases start by 24 (Kessler et al., 2005). Calming the brain early matters.
Can we make progress without medication?
Often, yes. Neurofeedback, PEMF, sleep, nutrition, movement, and co-regulation can shift the nervous system so skills stick. Some families also choose meds—both paths can complement each other.
How do I stop “rescuing” without causing a blow-up?
Pair calm validation with clear choices and tiny steps. Keep asks small; tie privileges to responsibilities.
Terminology
- Co-regulation: Your calm body helps your child’s body calm.
- Executive functioning skills: Brain skills for planning, starting, and finishing tasks.
- QEEG brain map: A data-driven look at brainwave patterns to guide care.
- Neurofeedback: Training the brain to self-regulate by rewarding healthier brainwave activity.
- PEMF therapy: Gentle pulsed electromagnetic fields that can help downshift a revved nervous system.
Citations
Kessler, R. C., Berglund, P., Demler, O., Jin, R., Merikangas, K. R., & Walters, E. E. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders. Archives of General Psychiatry, 62(6), 593–602.
https://jamanetwork.com/journals/jamapsychiatry/fullarticle/208678
Storch, E. A., Wu, M. S., Small, B. J., Crawford, E. A., Lewin, A. B., Horng, B., & Murphy, T. K. (2014). Mediators and moderators of functional impairment in adults with obsessive–compulsive disorder. Comprehensive Psychiatry, 55(3), 489–496. https://www.sciencedirect.com/science/article/pii/S0010440X13003180
Twenge, J. M., Joiner, T. E., Rogers, M. L., & Martin, G. N. (2018). Increases in depressive symptoms, suicide-related outcomes, and suicide rates among U.S. adolescents after 2010 and links to increased new media screen time. Clinical Psychological Science, 6(1), 3–17. https://doi.org/10.1177/2167702617723376
Always remember… “Calm Brain, Happy Family™”
Disclaimer: This article is not intended to give health advice, and it is recommended to consult with a physician before beginning any new wellness regimen. The effectiveness of diagnosis and treatment varies from patient to patient and condition to condition. Dr. Roseann Capanna-Hodge, LLC, does not guarantee specific results.
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!
© Roseann Capanna-Hodge