Estimated reading time: 9 minutes
One family-centered plan can turn chaotic days into calm, connected progress—starting with your child’s nervous system.
If your child’s behavior feels out of control lately, you’re not alone. As a clinician and mom, I see daily how ADHD in children can hijack home life, schoolwork, and everyone’s stress levels.
The good news? When we calm the brain first and work as a team, kids learn, connect, and thrive. In this guide, you’ll get simple, science-backed steps you can use today—without blame or shame.
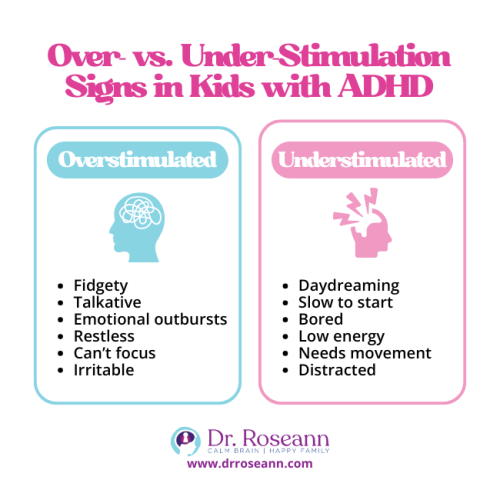
Why ADHD Looks Different From Day to Day
ADHD isn’t “bad behavior.” It’s a brain-based difference that affects attention, inhibition, and executive function skills.
When the nervous system is dysregulated, symptoms spike; when it’s calm, kids cope better. Behavior is communication. Let’s listen.
Key Takeaways
- Dysregulation ≠ defiance. Your child isn’t choosing struggle; their brain is overwhelmed.
- Symptoms shift with stress, sleep, and sensory load. That’s normal for ADHD.
- Parents are not failing. Strategies don’t work until the brain is calm first.
How to Start Treatment as a Family Without Overwhelm
Begin together. Behavioral parent training and caregiver education are first-line for younger children and a core part of care for all ages (Wolraich et al., 2019). Learn what to say, do, and track—then practice as a team.
Do This First
- Pick one routine to stabilize (mornings or homework). Keep steps visual.
- Use co-regulation techniques: slow breath, low voice, soft body.
- Log triggers and wins for two weeks. Patterns guide better support.
- Consider a qualified evaluation and school plan (504/IEP) early.
Parent story:
Marla’s 9-year-old melted down nightly over homework. She added movement breaks, a 10-minute “together start,” and a visual checklist. Within two weeks, blowups dropped from 5 to 1 per week. Takeaway: routine + co-regulation = fewer fires and more follow-through.
Daily Structure That Helps ADHD Brains Feel Safe and Succeed
ADHD brains love predictable structure. Think short steps, visible cues, and movement.
Build a Brain-Friendly Day
- Morning routine for ADHD: wake → water → movement → dress → breakfast → pack.
- Sensory breaks every 60–90 minutes: wall push-ups, trampoline, or a quick walk.
- Task chunking: 10–15 minute work blocks, then a micro-break.
- Positive reinforcement beats nagging. Spot the effort, not perfection.
Family Routine Builder
|
Situation |
What to Say (Calm Script) |
What to Do (1–2 Steps) |
Regulation Tool |
|
Morning rush |
“Let’s team up. First two steps together.” |
Hand the visual to the child; start with them |
3 slow breaths + shoulder squeeze |
|
Homework start |
“We’ll do 10 minutes, then a break.” |
Timer on; remove extra supplies |
Wall push-ups x10 |
|
Transition to bed |
“Time to land the day.” |
Lights dim; same order nightly |
Warm shower + story |
Behavior Tools That Actually Do and Don’t Work
Behavioral parent training improves parenting skills and reduces conduct problems. Effects on core ADHD symptoms are more minor but meaningful for family functioning (Rimestad et al., 2019).
Medication can help with attention and impulsivity. But skills and structure still matter (Cortese et al., 2018).
Use What’s Effective
- Clear expectations + visual rules
- First-then language: “First math, then Lego.”
- Choice within structure: “Two problems or three?”
- Reward effort; keep rewards immediate and small.
- Avoid: long lectures, inconsistent rules, or piling on consequences.
Parent story:
Mario’s 7-year-old grabbed toys from his sister. Parents posted 4 picture-rules and practiced “ask-and-trade.” Grabs fell fast; sibling play increased.
Takeaway:
Rehearse the replacement behavior, not just “don’t do that.”
“For preschoolers and younger kids, parent training in behavior management should be tried before prescribing medication.” — American Academy of Pediatrics, Wolraich et al. (2019).
How to Handle School—Ieps, 504s, and Real Classroom Supports
School success is a partnership. Ask for data, propose support, and keep it simple.
Classroom Supports That Work
- Front-row or low-distraction seating, movement breaks, chunked directions
- Visual schedule, extra processing time, reduced-length assignments
- Positive behavior plans with specific praise: “You started right away.”
Bring to Your Next Meeting
- Two weeks of behavior and focus data from home
- A short list of 3–5 accommodations that fit your child
- Your preferred communication plan (weekly email or checklist)
Parent story:
Amara’s 10-year-old couldn’t finish classwork. With chunked assignments and a quiet space, she completed 80% of her work on time within a month. Takeaway: fewer steps + fewer distractions = more wins.
Non-Medication Options That Are Worth Exploring
For some families, or alongside meds, non-medication ADHD treatments help regulation and learning:
- Neurofeedback and brain training protocols (evidence varies; discuss with your clinician).
- Body-based regulation: rhythmic movement, yoga, breathwork.
- Sleep, nutrition, exercise, and detox support for the nervous system.
- Co-regulation techniques you can use anywhere (slow breath + rhythm + warm tone).
- Sensory tools: weighted lap pad, noise-reducing headphones, chewable jewelry.
“Evidence supports stimulants short-term, but we must also invest in skills, school supports, and parent-led strategies.” — Cortese et al. (2018).
How Siblings and Co-Parents Can Stay Connected
ADHD can strain relationships. Protect your family system.
Protect the Team
- Weekly 15-minute huddle: what worked, what didn’t, one minor tweak.
- One-on-one time with siblings; rotate “special time.”
- Caregiver self-care: sleep, movement, and support group = more patience.
“Families matter. When parents feel competent and consistent, kids do better.” — Faraone et al. (2021).
How to Celebrate Progress and Keep Hope Alive
Kids need frequent wins to build motivation.
Make progress visible
- Goal boards with tiny steps
- Before/after stories: “Remember when mornings were tears? Look at you now.”
- Catch them doing right at least 5:1 versus corrections.
11 Family-Centered Strategies You Can Place on Your Fridge
- Educate the whole family about ADHD.
- Use a team approach at home and school.
- Practice open, judgment-free communication.
- Create a structured routine with visuals.
- Set clear expectations and keep them consistent.
- Use behavioral parent training strategies.
- Choose inclusive activities that everyone can enjoy.
- Lead with support and empathy.
- Protect caregiver energy with simple self-care.
- 10) Celebrate progress early and often.
- Connect with other parents so you remember you’re not alone.
From Struggle to Strength: Your Family’s ADHD Comeback Story
Every day you show up matters—even when it feels messy. When we see ADHD in children as a sign of a stressed brain, everything changes. We stop fighting our kids and start working with their brains.
This is where change begins—not in perfection, but in small, steady moments of calm.
A deep breath before reacting. A shared laugh after a hard day. A bedtime that finally ends in peace instead of tears.
These moments are proof: your child is capable of regulation, growth, and joy—and so are you. Keep leading with love, structure, and patience.
Calm the brain first, and the connection (and progress) will follow. Because when you regulate, your child learns to do the same. And that’s how families heal—one calm moment at a time.
Ready to Take the Next Step?
Grab my Quick Calm™ Mini-Course and discover simple tools that bring more peace to your evenings—starting tonight. Regulate. Connect. Correct.™
FAQs
How young can ADHD be diagnosed?
Preschoolers can be evaluated when symptoms are persistent and impairing. Early behavioral parent training helps regardless of the final diagnosis.
Do we have to choose between meds and skills?
No. Many families combine skills + school supports + lifestyle with or without medication. Meds can improve focus; skills build long-term independence.
My child masks at school but explodes at home—why?
Home is safe, so stress spills out. Focus on co-regulation, clear routines, and short, predictable transitions to lower the load.
Are screen limits really necessary?
For many kids, yes. Fast-paced screens spike arousal and sleep issues. Use screen hygiene: earlier cutoff, dim light, and a calming pre-bed routine.
Terminology
- Executive function: brain skills for planning, starting, and finishing tasks.
- Co-regulation: your calm helps your child’s nervous system settle.
- 504/IEP: school plans that add accommodations and special instruction to support learning.
- Behavioral parent training: coaching for caregivers on scripts, routines, and positive reinforcement.
Citations
Cortese, S., Adamo, N., Del Giovane, C., Mohr‐Jensen, C., Hayes, A. J., Carucci, S., Atkinson, L. Z., Zuddas, A., Barbui, C., & Cipriani, A. (2018). Comparative efficacy and tolerability of medications for attention-deficit hyperactivity disorder in children, adolescents, and adults: A systematic review and network meta-analysis. The Lancet Psychiatry, 5(9), 727–738. https://doi.org/10.1016/S2215-0366(18)30269-4
Wolraich, M. L., Hagan, J. F., Jr., Allan, C., Chan, E., Davison, D., Earls, M., Evans, S. W., Flinn, S. K., Froehlich, T., Frost, J., Holbrook, J. R., Kaplanek, B., Perrin, J. M., Pierce, K., Winner, J. D., & Zurhellen, W. (2019). Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics, 144(4), e20192528. https://doi.org/10.1542/peds.2019-2528
Rimestad, M. L., Lambek, R., Zacher Christiansen, H., & Hougaard, E. (2019). Short- and long-term effects of parent training for preschool children with or at risk of ADHD: A systematic review and meta-analysis. Journal of Attention Disorders, 23(5), 423–434. https://doi.org/10.1177/1087054716648775
Always remember… “Calm Brain, Happy Family™”
Disclaimer: This article is not intended to give health advice, and it is recommended to consult with a physician before beginning any new wellness regimen. The effectiveness of diagnosis and treatment varies from patient to patient and condition to condition. Dr. Roseann Capanna-Hodge, LLC, does not guarantee specific results.
Are you looking for SOLUTIONS for your struggling child or teen?
Dr. Roseann and her team are all about science-backed solutions, so you are in the right place!
©Roseann Capanna-Hodge